IVF

IVF (In Vitro Fertilization), also known as test-tube baby treatment, is one of the most advanced and effective methods of assisted reproductive technology (ART) used to help couples conceive when natural conception is not possible or has repeatedly failed.
In this procedure, a woman’s eggs are collected from her ovaries and combined with a man’s sperm in a specialized laboratory environment. After fertilization occurs and embryos are formed, one or more healthy embryos are transferred into the woman’s uterus to achieve pregnancy.
The IVF process typically involves several key stages:
Ovarian stimulation – Medications are given to help the ovaries produce multiple mature eggs.
Egg retrieval – The mature eggs are collected from the ovaries using a simple, minimally invasive procedure.
Fertilization – The retrieved eggs are mixed with sperm in the lab to allow fertilization.
Embryo culture – The embryos are monitored and grown in a controlled environment for several days.
Embryo transfer – One or more embryos are selected and placed into the woman’s uterus.
IVF can be recommended for various conditions, such as blocked fallopian tubes, severe male infertility, endometriosis, unexplained infertility, or when other treatments have not been successful.
Modern IVF techniques, such as ICSI (Intracytoplasmic Sperm Injection), PGT (Preimplantation Genetic Testing), and frozen embryo transfer, have significantly increased the success rates of treatment.
IUI (Intrauterine Insemination)

IUI (Intrauterine Insemination) is a type of assisted reproductive treatment in which prepared and concentrated sperm are directly placed into a woman’s uterus around the time of ovulation. The goal is to increase the number of sperm that reach the fallopian tubes and improve the chances of fertilization.
This method is simpler, less invasive, and more affordable than IVF, and is often recommended as one of the first-line treatments for certain fertility problems.
Steps of the IUI Procedure:
Ovulation monitoring: The woman’s ovulation cycle is tracked using ultrasound and hormone tests to determine the best timing for insemination.
Sperm preparation: A sperm sample (from the partner or donor) is processed in the lab to separate healthy and motile sperm from weaker ones.
Insemination: The concentrated sperm are gently injected into the uterus through a thin, flexible catheter.
Follow-up: After insemination, the woman may rest briefly, and a pregnancy test is done about two weeks later.
When Is IUI Recommended?
IUI is suitable for couples with:
Mild male infertility (low sperm count or motility)
Ovulation disorders
Cervical mucus problems
Unexplained infertility
Use of donor sperm
However, IUI may not be effective for women with blocked fallopian tubes, severe endometriosis, or for men with very low sperm count or quality—in such cases, IVF is usually recommended.
Overall, IUI is a simple, low-risk, and cost-effective fertility treatment that can significantly increase the chances of pregnancy for selected couples.
PGD
PGD-A, also known as PGT-A (Preimplantation Genetic Testing for Aneuploidy), is an advanced laboratory technique used during IVF treatment to analyze the chromosomal health of embryos before they are transferred into the uterus.
The goal of PGD-A is to identify embryos that have the correct number of chromosomes (euploid embryos) and to avoid transferring those with chromosomal abnormalities (aneuploid embryos), which could lead to implantation failure, miscarriage, or genetic disorders.
How PGD-A Works:
IVF and embryo culture: Eggs are fertilized in the laboratory, and embryos are grown for several days (usually up to the blastocyst stage, day 5–6).
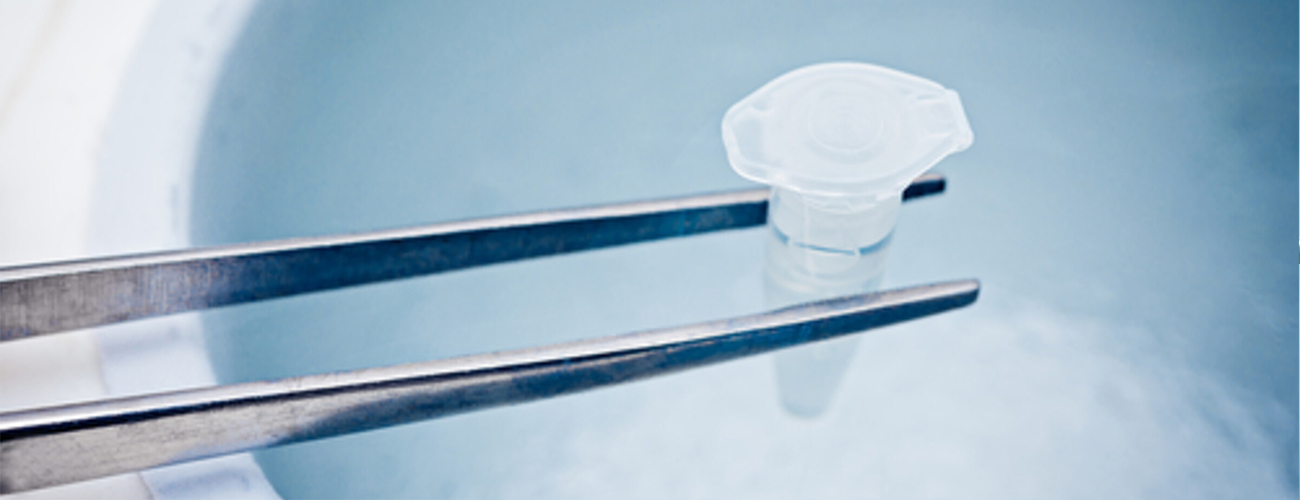
Embryo biopsy: A few cells are carefully removed from the outer layer of each embryo (the trophectoderm) without harming the embryo.
Genetic analysis: The sampled cells are analyzed using advanced molecular techniques (such as Next-Generation Sequencing – NGS) to check for chromosomal abnormalities.
Embryo selection: Only chromosomally normal embryos are selected for transfer to the uterus, increasing the chances of a healthy pregnancy.
Benefits of PGD-A:
Increases the success rate of IVF
Reduces the risk of miscarriage
Helps identify embryos with normal chromosomes
Improves the likelihood of a healthy baby
Reduces the time and number of IVF cycles needed to achieve pregnancy
Who Can Benefit from PGD-A?
PGD-A is especially recommended for:
Women aged 35 and older (higher risk of chromosomal errors)
Couples with recurrent miscarriage
Couples with multiple failed IVF cycles
Couples with a history of chromosomal abnormalities
Cases of severe male infertility
In summary, PGD-A is a powerful tool that allows fertility specialists to identify the healthiest embryos, improving the chances of successful implantation and a healthy pregnancy outcome.